Study design
Observational prospective study.
Study period
July 2018 to December2019.
Study population
FAST-positive patients admitted in study period at ATC PGIMER Chandigarh, India were included in the study as per the inclusion and exclusion criteria. Informed understood written consent was taken from all the patients and approval from the institute’s ethical committee was obtained.
Sample size
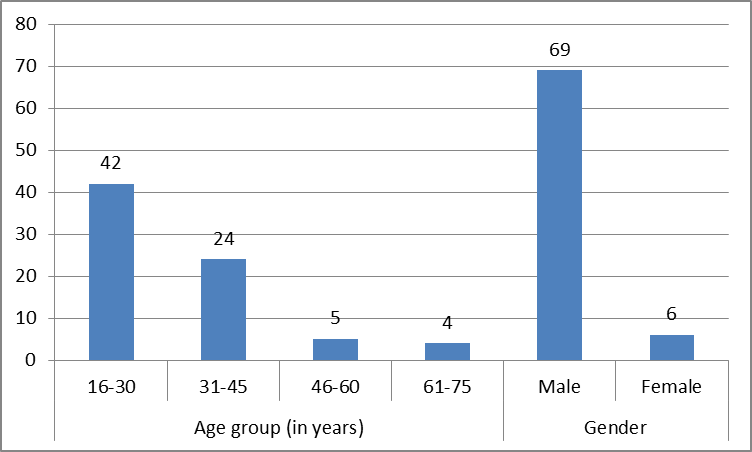
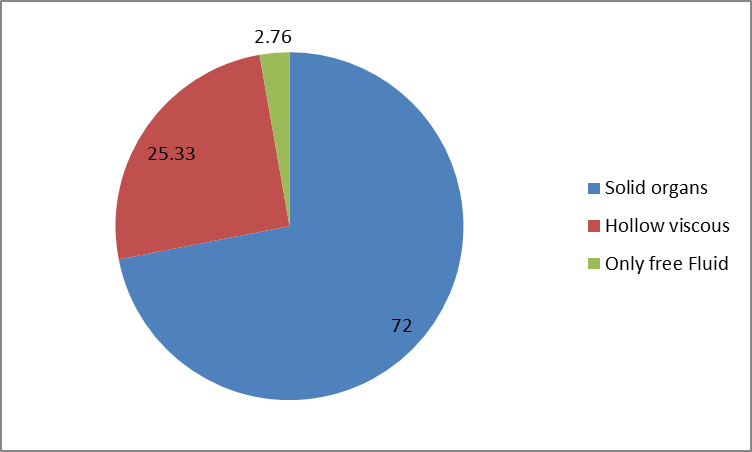
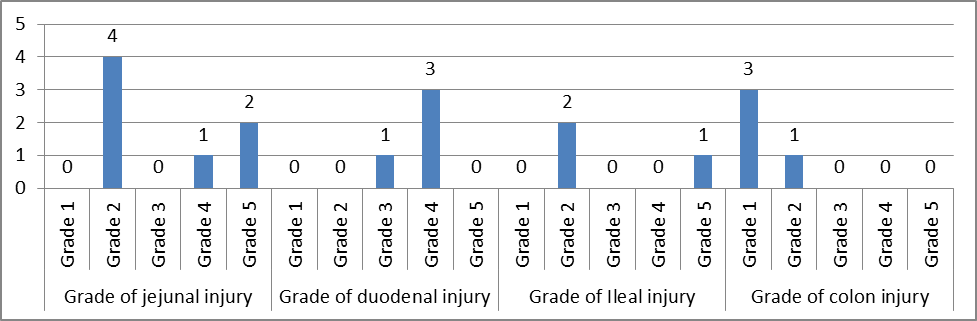
Seventy five consecutive patients were recruited based on satisfying the inclusion and exclusion criteria. All the recruited patient's injuries were classified according to existing classification of organ injury. Pattern, prevalence, non-operative versus operative management and outcome in term of mortality and morbidity were monitored.
Eligibility
All consecutive patients with blunt trauma abdomen admitted during the time Frame of the study.
Inclusion Criteria
All patients with blunt trauma abdomen having FAST POSITIVE or evidence of solid or
viscous injury clinically or radio logically.
Both Sex
Age >14 years and <80 years
Patients giving a valid informed consent.
Exclusion Criteria
Age <14 years as they are managed by department of pediatric surgery at PGIMER Chandigarh
Material & Methods
Advance Trauma Center PGIMER Chandigarh is the majortrauma center of India and it caters major population of Punjab, Haryana, Chandigarh, Himachal, Uttar Pradesh, and Bihar, J&K, Rajasthan and act as referral center for the urban and rural hospitals within the region. It has a computerized registry into which trained data collectors have prospectively entered data on all injury admissions. Patients admitted for Blunt Trauma Abdomen were taken into study and categorized into:
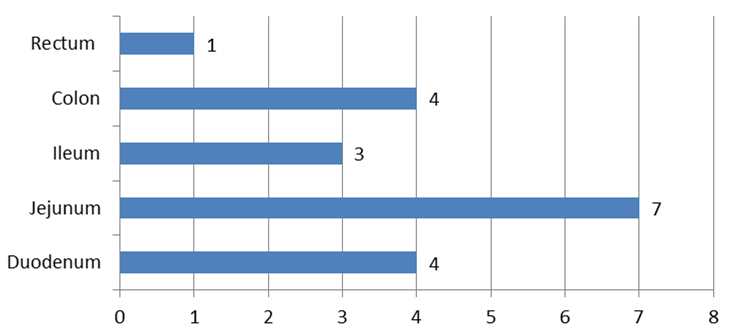
Patients with hollow viscous perforation
Patients with solid organ injury
Patients with solid and hollow viscous organ injury along with other coexisting injuries
Patients were managed as per existing protocol of trauma guidelines of the institute and ATLS guidelines and outcome in term of morbidity mortality and length of hospital stay was monitored. Operative, non-operative management and its indications and outcomes were evaluated.
Clinical course
Patients with blunt trauma abdomen were taken and their history was taken. Name, age, sex, residence, mode of injury, time of injury, time of arrival at ATC, brief history about antecedent incident was taken. Primary survey was done and GCS of patient and vitals such as pulse, blood pressure, respiration was noted. Airway, breathing, circulation was secured as per ATLS guidelines. Secondary survey was done, and detailed injuries were noted from head to toe.
After initial resuscitation patient underwent routine blood investigations such ABG, haemogram, blood biochemistry including electrolytes, renal function test and liver function test. Medico legal x-rays of skull with cervical spine, bilateral hip with pelvis, chest and abdominal X-ray was performed in addition injury specific x rays. FAST was done preliminary for BTA. In FAST positive patients CECT abdomen was performed and details of organ injured was noted. All the injuries noted clinically and by radiology were given an AIS and ISS score. Specific organ injuries were graded according to AAST grading of organ injuries.
Conservative or surgical management was done as per existing guidelines of institute. Conservative management includes BTA charting (hourly monitoring of pulse, blood pressure, respiration rate, urine output, abdominal girth, febrile status, 6hourly hemogram) transfusion of blood products, radiological interventions like percutaneous drainage or angioembolization, as guided by the clinical status of the patient, biochemical and radiological findings.
Surgical management for hollow viscus perforation and hemodynamically unstable solid organ injury includes exploratory laprotomy. Postoperatively, patient was monitored and managed according to clinical features, hemodynamic status with the help of biochemical and radiological investigations as indicated. Mortality and morbidity were noted
Statistical Analysis
Data were summarized and expressed as frequency and percentages. All calculations were conducted with standard statistical programs (SPSS 8.01, SPSS, Inc, Chicago IL).