Study Design, Settings and Participants
It was a hospital based cross-sectional study conducted over a period of one year from June 2018 to May 2019 in ophthalmology department of a tertiary care teaching hospital in Himachal Pradesh, India. All HIV-positive patients between 18 to 50 year of age group, registered at the ART centre and referred to Ophthalmology OPD for ocular complaints and asymptomatic patients from ART centre were selected randomly for the study. Patient with confounding factors and co morbidities like diabetes, corneal scars, lid abnormalities, contact wearers, SJS, arthritis, any other connective tissue disorder; patients who were already on treatment for DES, oral contraceptive pills, pregnant females and those taking any medications like antidepressants, antihistaminics, anxiolytics which can independently cause dry eye and seriously ill patients who were not able to cooperate for ophthalmological examination was excluded from the study. Total 346 HIV patients were examined but after considering inclusion and exclusion criteria 120 participants were finally included in our study. Every patient was on Highly Active Antiretroviral Therapy (HAART).
Data Collection
After taking written informed consent from the study subjects, data was collected in a predesigned, pre-tested, semi-structured interview schedule in which socio-demographic profile like age, gender, occupation, duration of ART, duration of disease etc were collected. After taking history as per proforma, each patient has undergone detailed ophthalmological examination in the following sequence.
Dry Eye Questionnaire - Ocular Surface Disease Index Score (OSDI)
OSDI questionnaire was administered to all patients and by a single examiner. To those who were non conversant in English, the questions were explained to the patients in their local language. The OSDI questionnaire has 12 items, with each question given a score ranging from 0 (none of the time) to 4 (all of the time). The final score was calculated by multiplying the sum of all the scores by 25 and then dividing the total by the number of questions answered. Scores range from 0 to 100 with 0–12 representing normal, 13–22 representing mild DED, 23–32 representing moderate DED, and ≥33 representing severe DED [7-8].
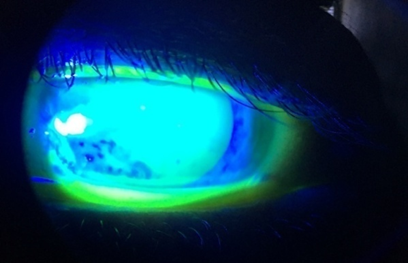
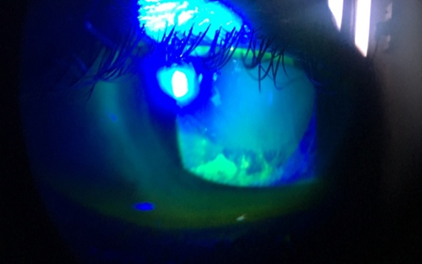
TBUT (Tear Film Break Up Time)
Tear break-up time was performed by moistening a fluorescein strip with sterile non preserved saline and applying it to the inferior tarsal conjunctiva. After several blinks, the tear film was examined using a broad beam of the slit-lamp biomicroscope with a cobalt blue filter. The time lapse between the last blink and the appearance of the first randomly distributed dark discontinuity in the fluorescein -stained tear film is the tear break-up time. Break-up times less than 20 seconds was considered abnormal. This procedure was repeated three times on both eyes [7-9].
Schirmer-1 Test Without Anesthesia
The Schirmer test was performed by placing a narrow filter-paper strip in the inferior cul-de-sac. Aqueous tear production was measured by the length in millimeters that the strip wets during the test period, generally 5 minutes. Test was performed with eyes closed. Serin et al., suggested that administering the Schirmer test with the patient’s eyes closed producesfewer variable results and greater repeatability [10]. While an isolated abnormal result can be nonspecific, serially consistent low results are highly suggestive of aqueous deficiency [8,11-12]. Severity grading was done as follows; >15 mm/5 min (Normal), 10-15 mm/5min (Mild Dry Eye), 5-9 mm/5min (Moderate Dry Eye) and <5 mm/5min (Severe Dry Eye).
Schirmers Test 1 With Anesthesia
The Schirmer test with anesthesia, also referred to as a basic secretion test, has been reported to give more variable results than the Schirmer test done without anesthesia. If topical anesthesia is applied, excess fluid should be gently removed from the cul-de-sac prior to insertion of the filter paper. This test is performed after 15 minutes of Schirmer’s test 1. After putting topical proparacaine drops, schirmer’s strip was applied as for Schirmer’s test 1. Results noted down after 5 minutes. <6mm/5min was considered abnormal and >6 mm of wetting after 5 minutes was considered normal.
Rose Bengal Staining
Rose Bengal staining was done and graded as van bitzerveld scoring. Rose Bengal score > 4 was considered abnormal and < 4 was considered normal. Maximum score was 9. Intensity scored in 2 exposed nasal conjunctival zones and cornea. It was started after putting anaesthetic drop to avoid irritation as this stain is slightly toxic to epithelial cells [7,8].
Posterior segment examination was also performed in every patient. Those patients who were found to have abnormalities other than dry eye were treated accordingly.
Statistical Analysis
Data were analyzed and statistically evaluated using SPSS software, version 17 (Chicago II, USA). Quantitative data was expressed in mean, standard deviation or median with interquartile range while qualitative data were expressed in percentage.
Ethical Issues
All participants were explained about the purpose of the study. Confidentiality was assured to them along with informed written consent. The study was approved by the Institutional Ethical Committee